This topic is brought to you by popular demand! I've had great deal of requests for a topic on total knee replacements or as we call them in the ortho world TKAs (Total Knee Arthroplasty). TKAs can seem overwhelming and downright SPOOKY if you are faced with the possibility of surgery. Let's see if we can dust some cobwebs off the common myths about TKAs and reveal the truth hidden underneath!
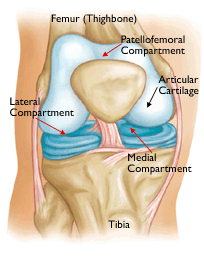
I have a conversation about the compartments of the knee with patients on a weekly basis, so this may sound familiar to some of you. The knee is separated into three compartments, the inside of the knee (Medial compartment) outside of the joint (Lateral compartment) and the knee cap joint (Patellofemoral compartment). The knee may wear in one, two, or all three of those compartments and the amount of wear determines what surgery is recommended.
There are two types of cartilage within the knee. The Meniscus the large shock absorber between the bones and Articular cartilage which covers the ends of the bones. Articular cartilage acts in a similar way to enamel on our teeth, it in itself does not feel pain, but when it is worn away the bone beneath feels pain. This is considered arthritis (just like a cavity in your tooth) and can be very painful.
When you have this break down in cartilage in one of the compartments in the knee that one area of the knee can be replaced. This is called a Unicompartmental Arthroplasty or "Half Knee." I personally think we should call them "1/3 knee replacements" but my opinion doesn't seem to count for much! The problem is when individuals begin to develop damage in two sometimes all three compartments of the knee. This is global or total knee arthritis, and is when surgeons recommend a TKA to replace the entire knee.
By the time a patient needs a total knee replacement it is usually easy to see on xray studies. As you can see on my background images for the blog the patients' knees are pretty healthy with good space between the thigh bone (femur) and shin bone (tibia). He did not need a TKA he was actually a young healthy teenager. In contrast, this knee shown below, has no joint space at all in the medial compartment, or "bone on bone" arthritis. The patient also has bone spurs that have formed at the ends of the femur and tibia at the joint line. The body will try to put down bone in areas where cartilage has been worn away. It is a protective mechanism in the body but unfortunately backfires and causes us to lose range of motion.

Total knee arthroplasties as we know them were developed in the early 1970s. The surgery continues to be tweaked and modified on a regular basis but many of the concepts are the same. We still replace the end of the femur and the tibia with metal components and a plastic spacer replaces the meniscus. There are many companies on the market today and most will tell you their knee components are the best around. I compare this to care manufactures. Many are built on similar constructs with different bells and whistles, but all will drive you from one place to another. I think the most important concept is that your surgeon is comfortable working with the implant. Most joint surgeons have a preferred brand or two that they feel works best for their patients and has had the best outcomes in their hands.

There are two major distinctions when it comes to total knee replacement implants--cemented vs press fit components. The type of component a surgeon uses often is related to where he/she was trained. A "press-fit" component get its name because it is actually impacted or pressed onto the ends of the bones. The idea is that the patient's own bone will actually adhere or grow into the metal components forming a stable construct. This is good for younger patients who may need a second replacement procedure early in their lifetime because revising these implants is a little easier. A cemented implant requires gluing or cementing the metal onto the bone. This also forms a stable construct, and may be good for older patients or patients with poor quality bone. The cement allows for a secondary fixation when poor quality bone may not be quite enough.
TKAs are a fascinating topic and relevant to so many people. I hope this provides a background on the procedure and need for a replacement. As I began writing this article it became clear that it would be too large for one post. We have so much more to discuss!! Hospital stays, rehabilitation, risks vs benefits of surgery. I will have to post a TKA Part Two in the near future. Feel free to ask questions if you would like them included in that article.
Next post in two weeks is a surprise...
For more info on TKAs check out the AAOS webpage here
Sources
Ranawat, C. (2002). History of Total Knee Replacement. J South Orthopedics Assoc, 11(4), 218-26. Retrieved September 22, 2015, from http://www.ncbi.nlm.nih.gov/pubmed/12597066
The information on this blog is intended for informational and educational purposes only. It is not intended to be used in place of medical advice. If you have orthopedic issues that need to be addressed please contact your physician.


